flu update: all your questions answered.
February 25, 2025: The newest developments are not moving in our favor.
Hi friends!
I was hoping to go a month or more before another flu post but after my latest round of reading up on the flu, I’m concerned about what I’m seeing as a microbiologist. (My last post from February 16 answers other questions but this post stands alone too.)
This is formatted to make it easy to skim so you can read what parts you want to read.
Why are you concerned?
So the latest news is that mice have officially picked up the HPAI (highly pathogenic avian influenza) strain referred to as H5N1. That’s bad.
But let’s back up a minute. H5N1 type of flu is a virus that was first identified in 1996 and despite some humans getting sick, it was a virus that didn’t demand much of our attention. About a year ago, we noticed that it had presented in cows for the first time and scientists reacted with a big Scooby Doo “ruh roh.”
Flu is already a rapidly evolving virus—that’s why the flu shot has a new formulation each year. But seeing H5N1 showing up in animals other than birds is a sign that it’s changing. Change is bad. In addition to cows, H5N1 now been found in tigers, polar bears, seals, cats, and dogs and is gradually getting better at adapting to new organisms.
Humans are also organisms. Ruh roh.
Humans have been infected with H5N1 but the crucial tipping point is when there is HUMAN to HUMAN transmission. It’s not happened yet. But I’m concerned this is getting close to being inevitable. That would launch a flu pandemic which could be pretty significant. We got lucky during the 2009 flu pandemic and it could happen again but we can’t count on it.
What about the mice?
The jump from mice to cows is significant band when I explained this to one of of my kids, he laughed out loud.
Mice most likely contracted H5N1 from drinking a puddle of unpasteurized milk in a milking barn or from being in contact with the dust from bird feces.
Unlike mice, sick cows or seals can’t show up in your living room one day and give you the flu. But mice can. Mice are small and known for their propensity to inhabit human spaces undetected.
Dairy and chicken farmers know they are at risk and can take preventative measures. But mice carrying H5N1 flu means more frequent and unannounced contact between infected animals and humans.
How will human to human transmission will happen?
It’s a math game. You know why casinos give out free drinks? The want gamblers to keep pulling that lever. Every time an organism gets H5N1 flu, it’s like pulling that lever one more time. The more times we hit that lever, the faster it happens. As of today, over 75% of dairy farms are infected with H5N1. While it won’t make our milk supply unsafe, that’s a LOT of flu levers.
Every time a viral particle replicates, there’s a teeny tiny risk that a small error is made copying it’s genetic material. A copy error of sorts. Most of the errors just render a viral particle ineffective. That’s call antigenic shift.
But there is also something called antigenic drift that happens. Nicola Lewis, Director of the Worldwide Influenza Centre at the Francis Crick Institute in London explains this as it pertains to pigs, “Flu viruses can also undergo what we call re-assortment, which happens when 2 different flu viruses infect a person or infect a pig at the same time. They shuffle their genetic material so that the progeny flu virus that comes out of the pig or the human is actually different.”
But it’s a numbers game and eventually one of those changes can cause human to human transmission. As we learned with COVID, that causes the roller coaster to begin and we are at the mercy of how prepared we are and how effective our public health leaders are.
What about regular flu?
On top of the risk of H5N1, regular seasonal flu is causing more deaths than COVID for the first time. Anecdotally, hospital coolers are full in a way that is reminiscent of 2020.
Unfortunately, the regular flu shot won’t do much for H5N1. It’s likely that it helps a non zero amount but not enough to be significant protection.
The main reason you may want to still get the seasonal flu shot is that it reduces hospitalization by over 80%. In many cases, it will prevent you from getting the regular flu at all. The CDC’s recently shuttered campaign made this point very effectively.
Is there a vaccine for H5N1 flu?
Yes and no. Practically speaking, it’s in the works. Big names like GlaxoSmithKline (GSK), Moderna, and Pfizer are all working on something. The good news is that we have a lot of knowledge about flu vaccines which wasn’t the case with COVID.
Canada’s main public health agency announced that it has secured a half million doses of GSK’s H5N1 vaccine to protect their most vulnerable citizens.
What is the US government doing right now?
The USDA is testing milk from dairy farms and publishing data. That’s valuable surveillance. NYC, a major international hub, is also typing all flu cases that pass through their hospitals. The more see what’s happening, the more we can respond appropriately.
The US has left the World Health Organization (again). This was done during the first Trump administration but due to the waiting period, Biden rejoined before any real damage was done. I would have thought that we learned very well from the COVID-19 pandemic that there is no way that you can isolate yourself from the world and be safe from the many health threats that don’t respect borders. Anything we do that diminishes our ability to not only collaborate, but collaborate efficiently with countries all over the world—regardless of whether we agree with them politically—to stop global health threats is really important. While we do contribute money to WHO, it’s entire budget is smaller than that of a single major US hospital. A truly excellent economic value especially after seeing what an economic nightmare a pandemic can be. Remember what happened to lumber?
Although I’ve not heard of any specific flu vaccine trials being axed by Elon Musk’s Department of Government Efficacy, there is concern that the broad cuts will slow down some elements of our avian flu response. Though they are working to rehire them, a few key Department of Agriculture employees working on avian flu were cut last week.
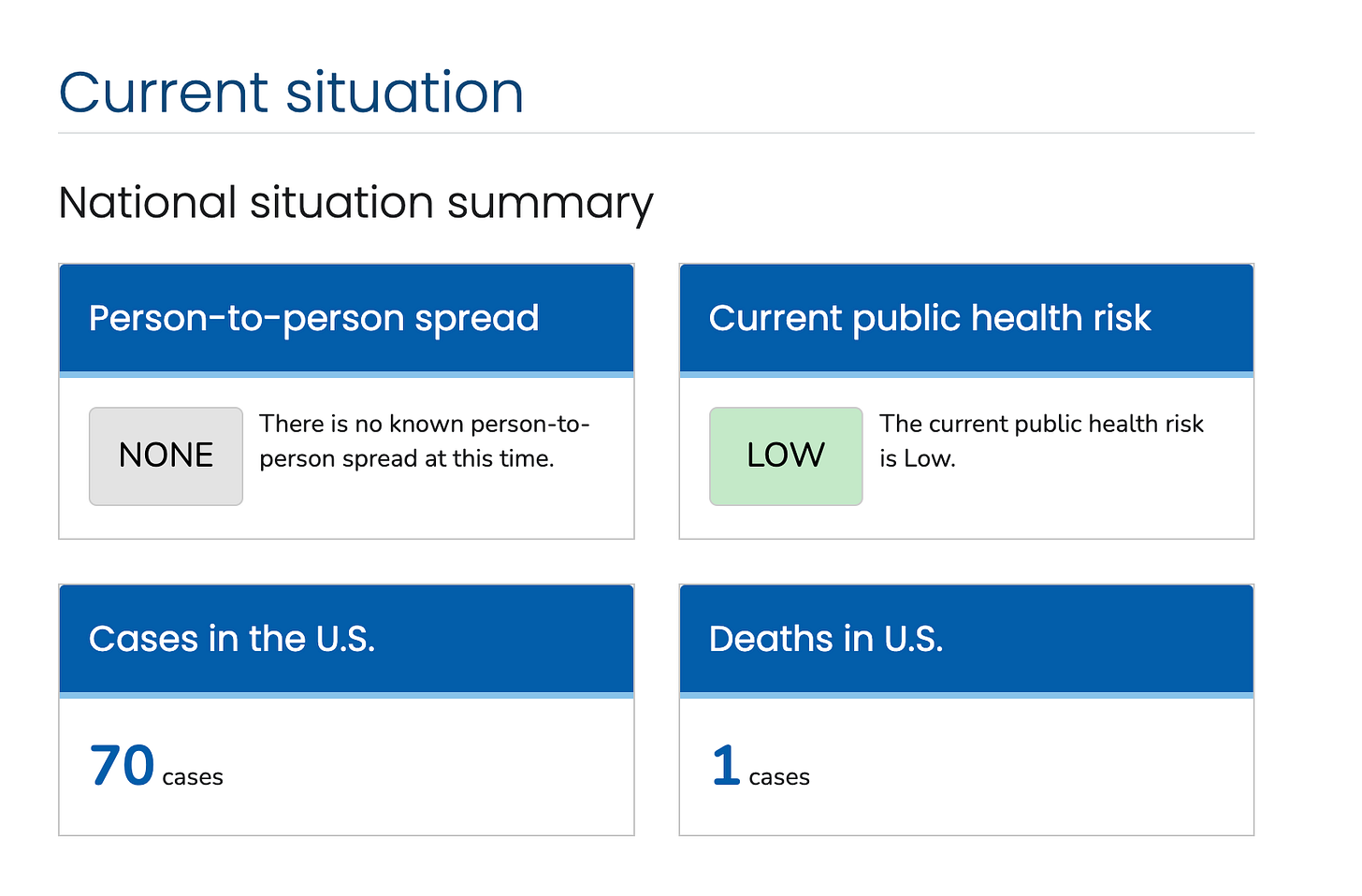
The Trump Administration has also changed how CDC reporting is issued. Though some reporting is back online, according to NPR, “The new results from the CDC are far from a real-time reflection of what's happening on the ground.” That said, it’s important for me to point out that the CDC current states that the avian flu risk to public health is low which is reassuring.
What should the US response be right now?
Increase surveillance of flu cases nationwide.
Thorough, frequent reporting of flu data.
Effective, easy to access communication with general public.
Determine if financial investment in planning makes sense for vaccines, PPE, testing, and contact tracing (including supplying at home test kits).
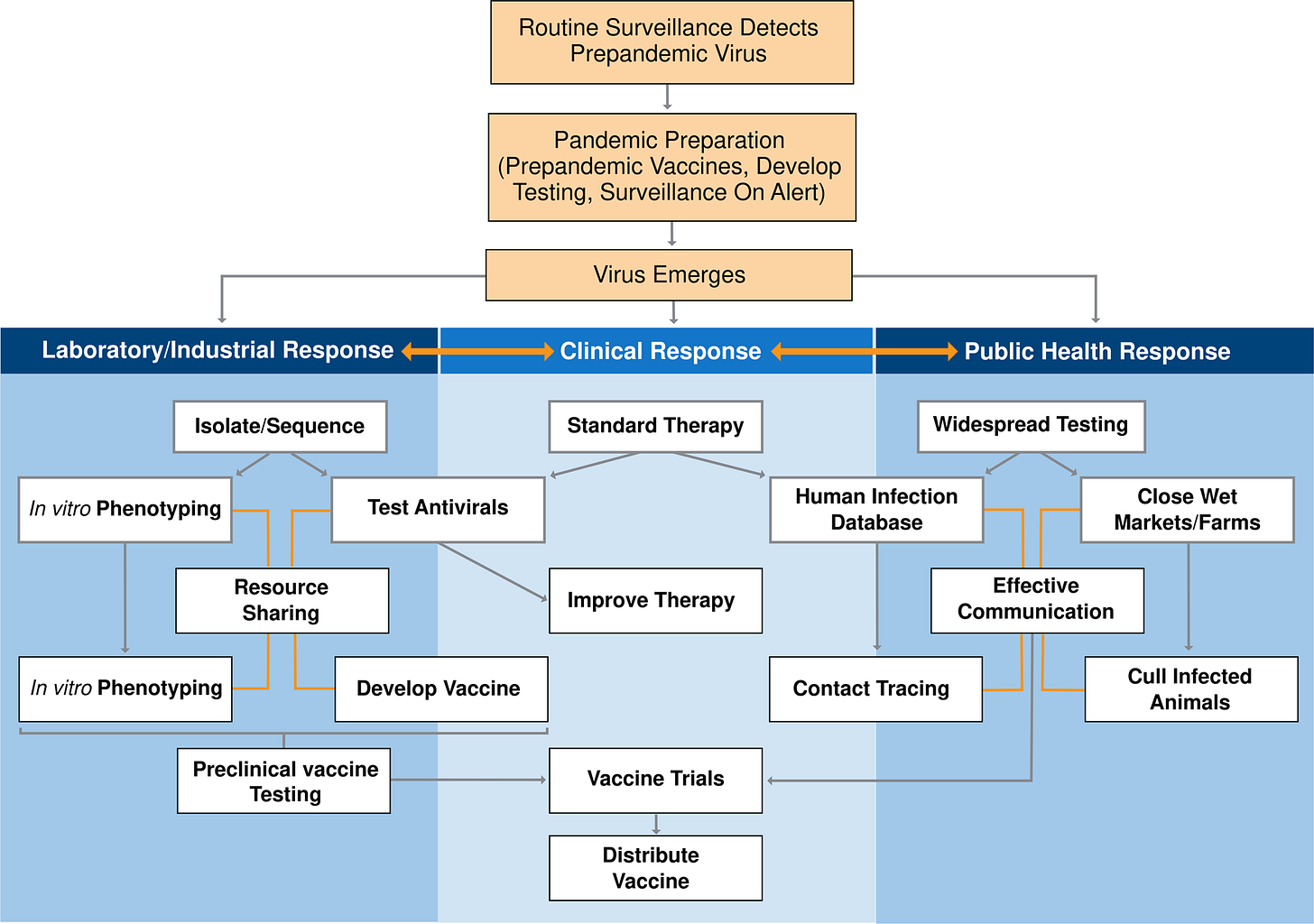
Though this is a bit fancy, here is what a good pandemic strategy looks like for my visual learners. It’s from a paper titled: “The evolution and future of influenza pandemic preparedness” and shows an ideal pandemic response.
Is it true that the H5N1 case fatality rate is 50%?
Yes and no. Based on current numbers based on less than 1000 people, yes. But that only counts the people tested and tracked. It doesn’t include the milder cases like the dairy farmers who tested positive for H5N1 antibodies and never remembered being sick.
The real number will be lower. 50% is an early number and assuming surveillance and data collection are effective, we’ll have a much more accurate number soon.
It’s going to be higher than the COVID case fatality rate which was roughly 1%. That does NOT mean you had a 1% chance of dying from COVID. An elderly man with emphysema is going to have a much higher risk of dying than a NCAA college athlete. It’s just a metric that helps us compare viruses.
We also don’t know what sort of mutation might cause human to human transmission. It could be a more or less severe form of the virus.
The case fatality rate will lower than 50% and higher than 1%. That’s all I can tell you for sure. Anyone who claims that the case fatality rate is going to be 50% is speaking too soon.
Any good news?
Tamiflu works for H5N1. That should not change. The short version is that the flu shot and Tamiflu work differently so Tamiflu is less susceptible to being rendered obsolete. As soon as you know you have the flu, tell your doctor so you can get started on Tamiflu. It reduces the severity of the flu and helps prevent complications, just like Paxlovid does for COVID. It’s reassuring that whatever happens with flu, we have a decent chance of starting off with a version of Paxlovid but for flu from day 1.
There are also relatively new at home flu test kits that will pick up avian flu. If your budget allows, having some of those handy would not be a bad idea. H5N1 will show up as Flu A on the at home tests. If you like Dr. Beachgem online, she has a great video that talks more about this.
I’m experimenting with nasal sprays and will have a review of those soon. While they aren’t as effective as masks, they do offer an extra layer of protection.
Speaking of tests, you can still get 4 free COVID test kits from the US government. Order them here.
Do you have any snarky comments for anyone?
Yes, thanks so much for asking!
I’m feeling concerned for the anti-vaxxers and anti-maskers right now. Nothing chances behavior more than a personal desire to survive. Eventually, there will be a tipping point where behavior will have to change. Otherwise, a pathogen will come along and the Darwin effect will help us course correct, if you catch my drift. Flu could do that and so could the emerging threat of measles.
Measles outbreak?!? Do I need to be concerned?
There is a outbreak in West Texas and surrounding areas that is growing. It’s still pretty concentrated in that geographic area but it’s a cause for concern due to how many people have been infected. Of the 100 or so infected, about 5 have been vaccinated—the rest unvaccinated.
Former Food and Drug Administration (FDA) Commissioner Scott Gottlieb said, “The risk to the United States right now is that a virus that has been largely extinguished from circulation in the U.S. could return and just continue to spread, even at a low level.”
Measles is super duper extra contagious. Scientists use a number called R0 to measure this. R0 is roughly equivalent to how many people get sick from one sick patient. For flu and COVID, that number is in the 1-2 range. For measles, it’s 12-18. It remains in the air for about 2 hours and good news—masks are effective prevention against the measles as it is airborne virus.
MMR vaccines provide immunity for LIFE so boosters aren’t necessary except in rare circumstances. If you know you you have gotten MMR in the past, you are all set—regardless of how bad things get.
According to the current vaccine schedule, kids get MMR at around 12-15 months and a booster at 4-6, typically before kindergarten. There is still a chance you can get the measles after vaccination but the case should be milder, less contagious, and drastically lower your risk of hospitalization. Which is good because 25% of patients are hospitalized.
People in the 70ish age group also should check with their doctors according to Dr. Céline Gounder, CBS News medical contributor and editor-at-large for public health at KFF Health News. She said "There is a very specific group that does have to worry about their immunity from vaccination. People born after 1957 but vaccinated before 1968 — that group is unlikely to have robust immunity from infection. At that point in time, they were using less effective vaccines." Anyone born before 1957 is likely to have been infected naturally and also has immunity.
Anything new?
All of my paid subscribers will have access to office hours this Sunday at from 7-8pm EST. Supporting my work means you are helping use your money to create the time I need in my schedule to make these posts happen as often as they are needed. As a chronically ill person, it makes a big difference. In exchange, for your support, I’ll make sure to answer any questions you have about what’s going on right now in public health.
That’s it for today. I’ll let you know if anything changes in the coming weeks! But for now, we continue to hope that the virus stays the same so we can focus on all the other things.
There has been an influx of new followers and I suspect that your little post hearts are a big reason why. If this post is helpful, give it a heart to help others find this info. Thanks!
Sources:
https://fortune.com/well/article/rfk-jr-cdc-cancels-flu-vaccine-campaign-amid-surge/
https://www.nature.com/articles/s12276-021-00603-0
https://publichealth.jhu.edu/2025/the-consequences-of-the-us-withdrawal-from-the-who
https://sph.umich.edu/news/2025posts/us-leaving-world-health-organization-now-what.html
https://publichealth.berkeley.edu/news-media/opinion/withdrawal-from-who-could-bring-tragedy
https://amp.cnn.com/cnn/2025/02/22/health/your-measles-questions-answered
https://www.cbsnews.com/news/measles-vaccine-booster-what-to-know/






The R0 for COVID was actually much higher. I’m not sure where you got that number from? I’ve seen reports of an R0 closer to 8 for COVID.
There’s also an ongoing TB outbreak in KS and now MO … which appears to be a mutation of the same areas outbreak in 2020-21
https://www.theguardian.com/us-news/2025/feb/06/kansas-tuberculosis-public-health