what, exactly, is so bad about severe MECFS?
Please proceed with caution when reading this post.
It’s extraordinarily challenging to explain what’s happening behind the scenes here with my health. But for my sake, I’m going to try.
Just a heads up before you read this post, especially if you are very close to me or you have a chronic illness yourself: this is going to be uncomfortable and touch on some extremely difficult topics related to living with chronic illness. Please proceed with caution. After a close friend read this, she offered some kind words that meant a lot to me:
"That was hard to read as someone who loves you, and yet, I would be mad at you for knowing this and not telling it.
Now it is a heavy thing we both know, and maybe it's a thought you can set down and let your community carry from time to time.”
Let me just cut to the chase: I’m much, much sicker than you probably realize I am. This is for a variety of reasons. First, MECFS is not well understood and unless you’ve taken the time to research it, you probably don’t know very much about it or where I fit into that picture. Second, I’ve been able to pretend I’m ok-ish for a long time. The struggle of living with MECFS is happening at home, where no one sees it except for me and my boys. Third, I think in the last year, I have gotten gradually worse.
Bedrest has taught me one thing: I definitely have severe ME
The viral infection that doctors believe triggered my MECFS occurred in 2006, when I was 20. About 10 years later (2016), I developed mild MECFS, about a 50% reduction in my activity levels. Around 2020, I spent a lot more time at home both due to COVID and slowly declining health. During this moderate MECFS phase, I was able to get on disability.
About 8 weeks ago, I noticed that my Fitbit data was telling me that I was overexerting my body pretty dramatically and embarked on Operation Bedrest to see what I could do to get that under control. It’s clear that I need to remain on bedrest for the foreseeable future.
The science is clear: MECFS patients must rest or else
Scientists don’t know which body system is malfunctioning in MECFS patients: the current contenders are mitochondrial issues, immune system dysregulation, neurological issues, gastrointestinal imbalance, or complex autonomic dysfunction. The one thing we do know is that the fastest way to worsen the health of a MECFS is overexertion.
New MECFS patients learn about staying within their “energy envelope.” Each person has a finite amount of energy to use per day. Healthy people can overdraw that limit, rest over the weekend, and not suffer beyond feeling run down. For MECFS patients, any overexertion or pushing beyond the energy envelope can cause a crash: a period of worsening symptoms. Crashes range from mild to severe and can take days, weeks, months, or even years to recover from. Many times, they are permanent.
The only possible path to recovery is to allow the body to rest.
Rest is very hard when you have MECFS
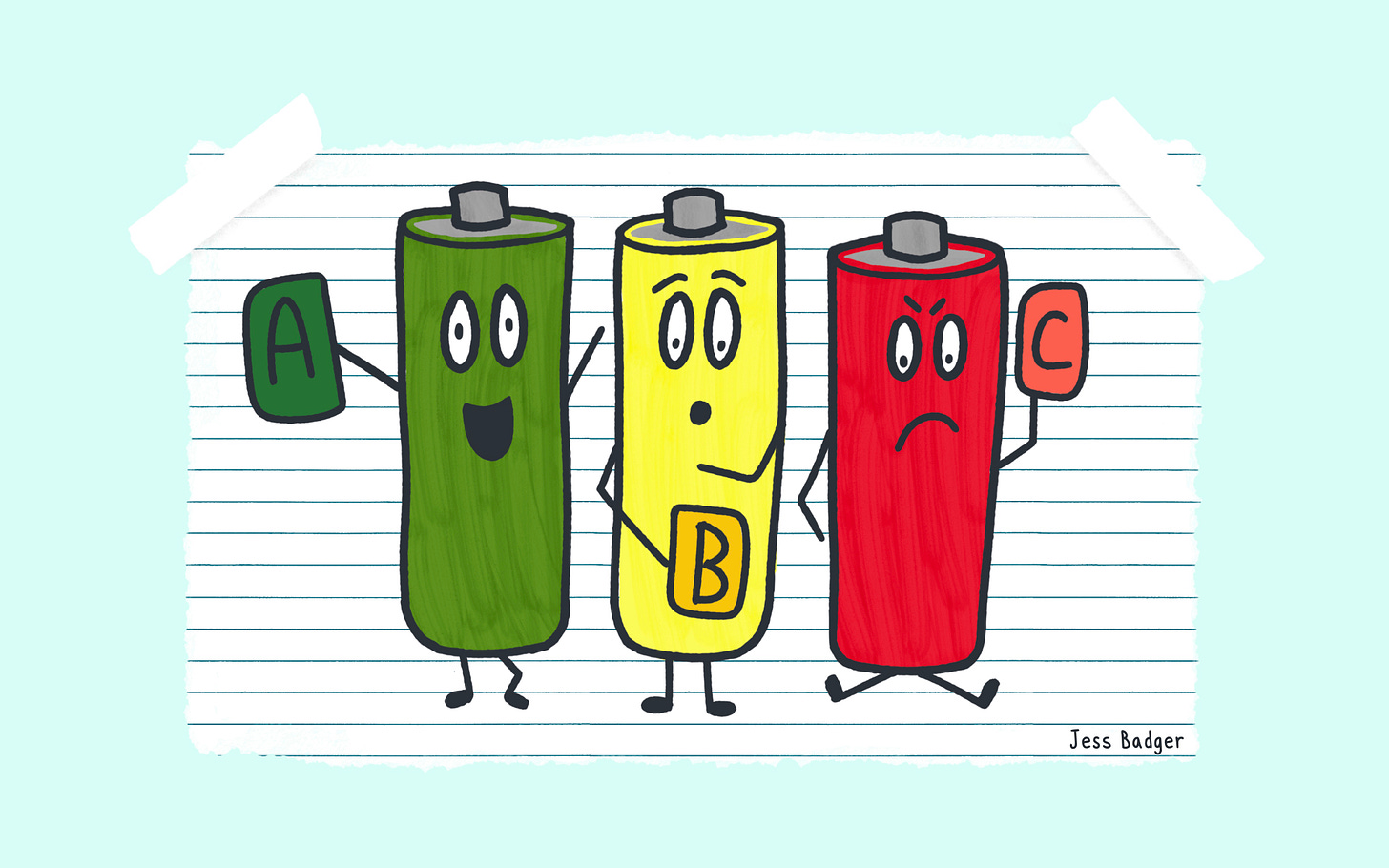
I’ve heard people use a battery analogy to understand MECFS. (This is not my analogy, it was originally created by Dr. Clark Elliott.)
Healthy people have 3 separate batteries: Battery A is charged up each night. Battery B is the backup battery: it runs your body but takes a bit longer to charge up and gets depleted more quickly. Battery C is the emergency battery: it only runs the most basic of life functions like eating or sleeping and it takes a very long time to recharge if it’s depleted.
People with MECFS don’t have Battery A at all. We are operating on Battery B all of the time. This explains why we can’t attend a doctor appointment one day and and grab lunch with a friend the next: we need time for the battery to charge. Our Battery B is the equivalent of a 5 year old iPhone with a charger that is loose. I might be able to get a little use out of it, but I also might try to use it to navigate home for about 10 minutes and watch it go from 90% to 10% charged.
We are running on Battery C basically all of the time and cannot rely on Battery B being online. Battery C can take weeks or months to charge back up again. Battery A and B are not able to be charged up or used at all until Battery C is back online.
I’m operating on Battery C and it’s unclear if it’s being charged
The whole point of Operation Bedrest was to see if I could get myself in a position where battery C was at minimum, charging up with that shitty, frayed charger that wiggles around.
You would think that would be an easy thing to know after eight weeks, but it remains unclear. I’m definitely not draining it as quickly but I do not know how much charging is happening right now. And that’s scary.
As it turns out, even with having two capable kids here part time, being alive requires tasks that take energy: prepping meals, taking showers, putting away groceries, keeping clothes clean, decluttering, and loading the dishwasher. Most everything else I can do from my bed.
The reality is I was overexerting myself before Operation Bedrest without realizing it. I was doing so little, it didn’t actually occur to me that I was doing “too much.” After all, I have to eat. What was I supposed to do? Not cook and eat food? Figuring out how to make sure Battery C is charging means I have to question literally every single movement my body makes. Every minute of everyday is consumed by this.
I have to get to the point where I’m absolutely positive I’m charging Battery C again or I will just get worse. So that’s why bedrest must continue and why I have to hire someone to help me around the house.
MECFS is unique in this way, usually exercise and movement are helpful. Which is why it would be really wonderful to understand why our bodies are responding this way.
The best case scenario: being able to access Battery B
If I can continue to rest as aggressively, then maybe after a few months, Battery B becomes usable. I don’t care about Battery A at all—I haven’t had one of those in over 10 years, I wouldn’t know what to do with it anyway.
Once we get to Battery B, then I can use it sparingly and just live a very slow-paced, gentle life mostly from my home to prevent any crashes.
But I’m perfectly ok with that as a long term plan, though I admit it is not what I would have chosen for myself.
The worst case scenario: very severe ME
If Battery C doesn’t get itself together, there is a good chance that I could see myself progressively worsen. It’s also possible that I could deal with a crash that causes a rapid drop in my ability to function.
While I have a lot of control over my ability to avoid crashes, I cannot avoid all of them. For people with severe MECFS, even a hours long trip to the emergency room can cause a crash. I got a filling this week and was too physically tired to shower or make dinner for the kids.
Currently, I don’t know how to rest more than I already am but what control I do have, I plan to use.
A note about seeing doctors
You might be thinking: why not talk to all the doctors about how to make sure you are charging your batteries properly? Unfortunately, there is not any current medical test or treatment for MECFS. There are very few specialists in the United States. That link includes a total of four specialists in NC. One is retired, two are no longer working at the practice, and I’ve seen the last one within a year. It cost me $800+ out of pocket (not reimbursable) and other than taking notes, there wasn’t much he could do for me.
I am continuing to keep my eye on both research progress and possible clinicians who can help me but let me be explicitly clear: the lack of medical support out there for patients with ME would flabber your gasters. The patients themselves have much more information about this condition that the medical professionals. Patients actually drive a lot of the research progress that does exist: one of the largest funders of MECFS research, Open Medicine Foundation, grew out of a mother trying to help her daughter. A prolific researcher named Ron Davis is the father of well known patient Whitney Dafoe.
Let’s look at the challenges of severe ME
Look, I don’t want to do this either but we are going to anyway. I'm very familiar with mild to moderate MECFS. I was added to a group just for the 25% of people with severe MECFS a few weeks ago and it’s been very enlightening. While I knew some of these things, it’s another animal to read about them knowing you are a part of that group.
It’s not unlike coming out as queer and reading the same articles about what society is doing to queer people: it just hits differently.
As a refresher, there are almost 1 million Americans with severe MECFS which means there are about 1 million Americans also dealing with these challenges. Many more are dealing with long COVID, an incredibly similar condition. Keep that in mind as you read this list: it’s not just a me thing.
It was a rough week on this group, including a death announcement for a long time member. Here are some of the challenges that other severe MECFS patients are dealing with based on their posts in the forum:
Unable to sit up in bed at all
Unable to stand for any length of time
Progressive cognitive decline
Require full time caregiver (unable to live independently)
Unable to tolerate other people speaking, sound, smells
Unable to listen to music, watch TV, or read
Unable to chew food
Unable to talk
Complications from lack of preventative care like dental infections and loose teeth
Crashes from ER visits or doctor appointments
COVID infections causing worsening baseline function
Unique form of depression due to being so isolated, grieving their former life, anxiety from being consumed by their illness, the stigma of the illness, and not having medical providers who can help
In addition, severe MECFS patients experience:
Suicide risk over 7 times the normal rate (specifically not linked to depression which I find fascinating)
Worsening symptoms such as starvation as their body shuts down and organs get to tired to work
Reduced life expectancy by about 20 years with leading causes of death suicide, cardiovascular issues, and cancer
Patients using MAID (medical aid in dying) to end their lives to avoid additional pain and suffering like Judith Schossböch did last week
Morbidity of secondary health issues that they cannot have treated adequately due to being bed bound at home
An “existential choice” of risking a crash by seeking medical or risking a worsening illness by not seeking medical care
Doctors who do not believe patients are sick and do not provide adequate medical care.
I simply cannot stress this last one enough. I regularly run into providers who tell me that I need to exercise more and go to therapy because my illness is being worsened by my “unhelpful mindset.”
Just in case you don’t believe me on that…
If that sounds like I’m catastrophizing a wee bit, it’s really important for you to understand that I’m actually downplaying the horror.
A woman in the UK named Maeve Boothby-O’Neill (27) died in 2021 of MECFS after the NHS repeatedly refused to treat her for malnutrition. She was too fatigued to eat and drink any longer. There was an formal inquest into her death and those involved believe that she would have had a chance of improving had she received appropriate medical care. There are no specialized units equipped to treat patients with severe MECFS and furthermore, “the inquest has also been told about a culture of disbelief among some senior NHS professionals who believed MECFS is a mental and not physical illness.”
And the UK is actually doing better overall with care for MECFS patients. It’s even worse in the United States in terms of doctor education and specialty care.
If I got breast cancer (knock on wood), I would be able to chose between specialists at 3 major hospitals around me. I would be tested and begin treatment. I would be presented with several options: if Plan A didn’t manage the cancer, we would move to Plan B. If none of the treatments successfully treated the cancer, I might be eligible for a drug trial. At the very least, I would be placed on hospice care and provided with comfort measures at the end of my life. Other doctors would know about my disease and how best to care for me.
Instead, I have MECFS. There is one specialist within 5 hours of where I live who cannot help me. I feel grateful that my primary care doctor has actually heard of my medical condition. I have been harmed by over a dozen providers in my life, many of whom recommended exercise which has significantly worsened my condition. I’m left to talking to other patients and Google Scholar to get guidance about what to do. If I need emergency care, I cannot count on a doctor knowing what my condition is or the best course of action. If anything, it pretty likely they will treat me like I’m psychologically disturbed vs. physically ill. The chance that I will crash by just seeking care is significant: and there are no measures to prevent that like planned hospital admissions or at home appointments. If I get very severe and was toward the end of my life, there is nonzero chance I might not even get nutritional support.
So now what?
We prepare for the worst and hope for the best.
Gotta work on Battery C above all else: there are no shortcuts and there is very little wiggle room. Obviously, the stakes feel very high. My plan is to rest as much as humanly possible and accept all the help I can right now.
I’m lucky that I have a incredible therapist who is enormously supportive. I also have a primary care doctor who is providing excellent care too.
My therapist was trained as a social worker and helped me come up with this list of things we can work on in the coming months to ensure I have as much support in place as possible.
Hiring a home health worker
Thinking strategically about home accessibility to enable greater capacity to move freely in the home (or a longer term plan to move to a more accessible home)
Reviewing medications to ensure there are no meds that might be worsening symptoms or trying new meds that might improve symptoms
Increasing communication between providers
Creating a timeline/list of past medical conditions/diagnoses/symptoms, when they started, their severity, and any treatment that were tried (and what worked/didn't) as well as list of current symptoms/disability level
Possibly seeking out additional providers to add to treatment team
Exploring ways to receive medical care at home
Ruling out differential diagnoses, just in case this isn’t MECFS
Continuing to monitor data from wearables to pace effectively (I ordered an Oura ring for Christmas after hearing one too many rave reviews from a close friend whose ring predicted her cold and kidney infections before she noticed symptoms herself.)
Exploring this website: https://direct.rthm.com/treatment-summary
Final thoughts
So that’s what I’m dealing with. There is no easy way to wrap this up into a nice little conclusion. This the reality in all it’s messy glory and it’s important to me that we are all on the same page.
Sometimes I joke that “it’s a miracle that I’m cheerful and sane” as I lay in bed all day. This is why. It’s genuinely depressing, awful, miserable disease that dominates every single waking hour. Hell, I dream about overexerting so it even dominates even my sleeping hours.
I have to admit I have a little chip on my shoulder about this. I saw what happened to people during COVID. The pandemic asked people to stay home and entertain themselves. It caused them to go stir crazy and claw up the walls in frustration while their mental health suffered.
This is that but jacked up several notches and with no end in sight. I’m convinced you couldn’t even pay people to do this for more than a few weeks. I’m a bona fide professional and don’t feel like I get nearly enough credit for that most days.
On on top of that there is a lot of pressure to not talk about it because it makes other people uncomfortable. I have every reason to be angry, bitter, and resentful. But somehow, I’m still showing up for my kids and taking care of myself while facing all this head on. That’s something I am proud of.
I don’t know what the future holds. Maybe I can pull this off and stabilize that battery for several decades—no one knows. But I need to mentally prepare for a range of outcomes because I can only control so much, even with a positive attitude.
And it felt pretty important to tell you all of this so we are on the same page.
P.S. While I certainly don’t avoid talking about the hard topics, not all of my essays are this existential. Sharing my stories with you is a a privilege and one way you can provide comfort right now is signing up for updates below.
This post was the most difficult one to write and send out so your support in the form of comments, hearts, and subscribes are part of what is getting me through right now. Thank you so much.




Thank you for writing this—I greatly appreciate the chance to understand better what life impacts MECFS has. As a cancer survivor, the comparisons/contrasts do hit home for me. I know a bit about EDS, and where it leaves a person when all the doctors don’t know or don’t believe. Your writing and insight bring so much to all of us - I’m rooting for you 🧡
Thank you for sharing this.